TESTOSTERONE PROPIONATE INJECTION
General Information
TESTOSTERONE PROPIONATE INJECTION was the first successfully synthesized anabolic steroid. Testosterone propionate is a fast-acting, short-ester, oil-based injectable testosterone compound commonly prescribed for treating hypogonadism – low testosterone propionate injection levels and various related symptoms in males.
During a series of experiments in 1935, This testosterone propionate injection was first described 1935 to increase synthetic testosterone’s therapeutic usefulness by slowing its release into the bloodstream. Schering AG in Germany released it for clinical use two years later and featured it in a hybrid blend with testosterone enanthate under the brand name Testoviron. This was also the first commercially available version on the U.S. prescription drug market and remained the dominant form of testosterone globally before 1960.
Testosterone is the primary androgen found in the body. The testis, ovary, and adrenal cortex cells synthesize endogenous testosterone. Therapeutically, testosterone is used to manage hypogonadism, either congenital or acquired. Testosterone is also the most effective exogenous androgen for the palliative treatment of breast carcinoma in postmenopausal women. Testosterone was in use in 1938 and approved by the FDA in 1939. Anabolic steroids, derivatives of testosterone, have been used illicitly and are now controlled substances. Like many anabolic steroids, testosterone was classified as a controlled substance in 1991.
Testosterone is administered parenterally in regular and delayed-release (depot) dosage forms. In September 1995, the FDA initially approved testosterone transdermal patches (Androderm); many transdermal forms and brands are now available, including implants, gels, and topical solutions. A testosterone buccal system, Striant, was FDA-approved in July 2003; the system is a mucoadhesive product that adheres to the buccal mucosa and provides a controlled and sustained release of testosterone. In May 2014, the FDA approved an intranasal gel formulation (Natesto). A transdermal patch (Intrinsa) for hormone replacement in women is under investigation; the daily dosages used in women are much lower than for products used in males.
The FDA ruled in late 2004 that it would delay the approval of Intrinsa women’s testosterone patch and has required more safety data, especially cardiovascular and breast health. The Propionate Ester: An ester is a class of organic compounds that react with water to produce alcohols and organic or inorganic acids. Most esters are derived from carboxylic acids, and injectable testosterone is typically administered with one or multiple esters.
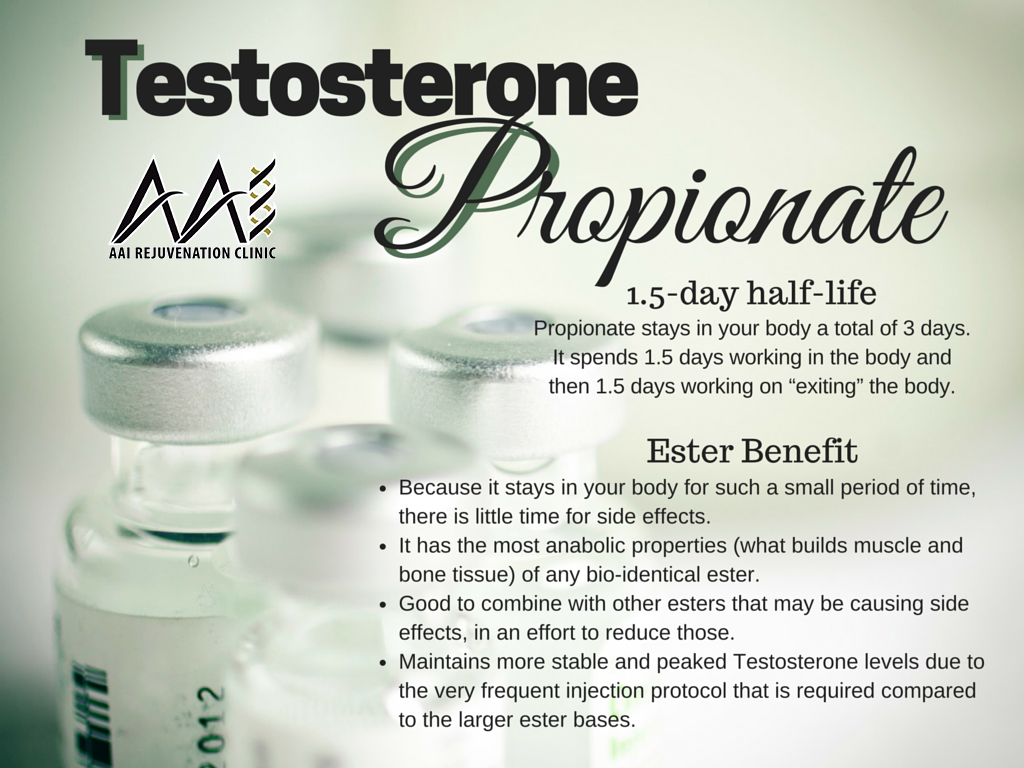
Adding a carbon chain (ester) attached to the testosterone molecule controls how soluble it will be once it’s inside the bloodstream. The larger the carbon chain, the longer the ester, and the less soluble the medication; a large/long ester will have a longer half-life. The inverse is true of short carbon chains, like the propionate ester, which acts rapidly upon the body and evacuates the body at a similar rate. With a three-carbon chain, the testosterone ester possesses the shortest half-life of all testosterone esters at four days.
Mechanism of Action Endogenous testosterone is responsible for sexual maturation at all stages of development throughout life. Synthetically, it is prepared from cholesterol. The function of androgens in male development begins in the fetus, is crucial during puberty, and continues to play an important role in the adult male. Women also secrete small amounts of testosterone from the ovaries. The secretion of androgens from the adrenal cortex is insufficient to maintain male sexuality.
Increased androgen plasma concentrations suppress gonadotropin-releasing hormone (reducing endogenous testosterone), luteinizing hormone, and follicle-stimulating hormone by a negative-feedback mechanism. Testosterone also affects the formation of erythropoietin, the balance of calcium, and blood glucose.
Androgens have a high lipid solubility, enabling them to enter cells of target tissues rapidly. Within the cells, testosterone undergoes enzymatic conversion to 5-alpha-dihydro testosterone and forms a loosely bound complex with cytosolic receptors. Androgen action arises from the initiation of transcription and cellular changes in the nucleus brought about by this steroid-receptor complex. Normally, endogenous androgens stimulate RNA polymerase, resulting in increased protein production.
These proteins are responsible for normal male sexual development, including the growth and maturation of the prostate, seminal vesicle, penis, and scrotum. During puberty, androgens cause a sudden increase in growth and development of muscle, with redistribution of body fat.
Changes also occur in the larynx and vocal cords, deepening the voice. Puberty is completed with beard development and growth of body hair. Fusion of the epiphyses and termination of change is also governed by the androgens, as is the maintenance of spermatogenesis. Exogenous androgens are necessary for normal male growth and development when endogenous androgens are unavailable.
**NOTE** The content in this blog is subject to interpretation and is the opinion of the content writer. We do not claim it to be fact. We encourage you to consult a medical doctor before taking any prescribed medications or supplements.
Conclusion
Supporting Hormones health is essential for overall well-being and vitality. By incorporating regular exercise, proper nutrition, adequate sleep, stress management techniques, and IV therapy, you can help maintain optimal testosterone levels and lead a healthy, balanced life. Always consult a healthcare professional before making significant changes to your lifestyle or starting any new treatments to ensure they suit your needs.
At AAI Rejuvenation Clinic, we advise anyone to think seriously about beginning Hormone treatment if there is no medical need for it. However, we will take every precaution to ensure that you read your program’s positive benefits by providing the latest at-home hormonal mouth-swab testing to ensure we are continually monitoring your progress and aware of any adverse side effects. Fill out the Medical History Form, or if you need more information, call us at (866) 224-5698 or (866) AAI-Low-T.
Low Hormone Symptoms
- Motivation
- Sex Drive and Desire
- Depression
- Fatigue
- Erectile Dysfunction
- Cholesterol
- Low Energy
- Memory Loss
- Osteoporosis
- Wounds & Illness
- Muscle Mass
- Sleep Disturbances
- Thyroid Dysfunction
- Weight Gain
]]>