Why Is Testosterone Post Cycle Therapy Is Need It?
Why is Post Cycle Therapy (PCT) the most critical aspect of testosterone use? Post-cycle therapy (PCT) only existed in the late 1980s and 1990s, and only partially understood the mechanisms by which Testosterone affected the body during the 1950s, 1960s, and 1970s. During this period, doctors, scientists, and testosterone injection users were only beginning to learn about testosterone dynamics and how they affect the endocrine system. Since the beginning of testosterone injections, we believed and understood that administering Testosterone triggered the body’s negative loop of the (HPTA) Hypothalamic Pituitary Testicular Axis. That endogenous Testosterone production would result in being suppressed and shut down.
Unfortunately, during the early periods of testosterone use between the 1950s and 1990, there was limited access to the compounds or knowledge of effectiveness.
Today it is a very different story. The scientific and medical understanding of bio-identical testosterone use has soared exponentially since the old ‘golden era’ days of looking young and testosterone therapy use in athletics. Countless developments of beneficial compounds for hormonal recovery after testosterone therapy use, alongside the increased scientific and medical knowledge, have enabled testosterone use and its associated endocrine disruptions—the proper knowledge on how to recover the bodies from Hypothalamic Pituitary Testicular Axis (HPTA).
Through post-cycle therapy (PCT), we can not only emerge from their testosterone therapy while holding on to almost all of their benefits, but they can also increase the chances upwards to 90 percent or a higher range of emerging with a fully healthy (HPTA). After using exogenous testosterone injections, most users will experience a hormonal crash or post-cycle therapy crash, a physical environment in which vital essential hormones have been suppressed or shut down. The critical hormones in question are Luteinizing Hormone (LH), Follicle Stimulating Hormone (FSH), and subsequently (and most importantly), our natural Testosterone.
The Luteinizing Hormone (LH), and the Follicle Stimulating Hormone (FSH), are known as phototropism. These hormones increase Testosterone secretion. Also, alongside low levels of these hormones, to balance the essential hormones that have been thrown off balance, whereby will trim testosterone levels, and most of the time, depending on the factors, estrogen levels will be higher than usual, and levels of Cortisol a steroid hormone that destroys muscle tissue. With testosterone levels low and Cortisol levels on average or high, Cortisol can now become a threat to the new muscle during the new testosterone therapy.
(“Testosterone correctly suppresses and counteracts Cortisol’s catabolic effects on muscle tissue”).
The SHBG (Sex Hormone Binding Globulin) is also concern here, a protein that binds to sex hormones. Testosterone renders them inactive, essentially ‘handcuffing’ them and preventing them from exerting their effects. SHBG will also usually be elevated during the post-cycle therapy weeks due to the supraphysiological levels of androgens from the new testosterone therapy.
The human body will generally restore this imbalance of hormones and recover from testosterone levels on its own, over time, with no outside assistance or post-cycle therapy (PCT). Still, studies have shown that this will occur throughout one to four months without the intervention of testosterone-stimulating agents. Therefore, all testosterone therapy should be concerned with the fastest possible hormonal recovery, assisted and boosted with the use of Testosterone producing compounds correctly, also the attempt to allow the body to recover on its own from a very high probability of long-term endocrine damage to the Hypothalamic Pituitary Testicular Axis (HPTA), whereby the individual will develop-induced hypogonadism to inability the production of proper levels of Testosterone to rest.
So therefore paramount that an appropriate post-cycle therapy that includes multiple recovery compounds be utilized to restore the (HPTA) function and normalize the levels as quickly as possible. To avoid any potential permanent damage, which can take priority over maintaining the recently gained muscle mass and any other benefits.
What Post Cycle Therapy Protocol?
There are many different types of post-cycle therapy (PCT) protocols that have overdeveloped over the years; any individual will become extremely confused about how many different opinions exist among the testosterone community; this article will present the best possible and most efficient post-cycle therapy protocol valid scientific data, also myths in regards to post cycle therapy (PCT), and outline which post cycle therapy (PCT) protocols should not follow due to recent more advanced developments, as well as contemporary better scientific and medical understandings of how a proper post cycle therapy protocol should work. At this point, there still exists very obsolete – and subsequently ineffective – post-cycle therapy (PCT) contracts that many testosterone users still utilize, and this presents a severe hazard not only for the individual unknowingly using a post-cycle medicine.
For example:
There are several therapeutic and safety reasons why you should not continue with testosterone injections indefinitely without giving your body time to normalize to reset. Because of the decline in benefits after six months of testosterone therapy, physicians need to regularly incorporate a cleanse therapy post cycle therapy (PCT) in an attempt to reactivate the endocrine in the body as you increase your testosterone levels using any testosterone therapy, now the levels of Testosterone circulating the body will shut down the natural production of your endogenous Testosterone; and also increases the production of Estrogen in your body, which can lead to a series of undesirable and unwanted side effects in the body. `
This means the synthesis of (LH) luteinizing hormone in your body; your brain produces this hormone to stimulate testosterone production. And follicle-stimulating hormone in the body, the hormone your mind makes to boost sperm production, suddenly stops. When Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) levels are no longer detectable, your body will not experience the exceptional health benefits and energy-optimizing results expected from a testosterone injection program. Another critical concern for men is testicular atrophy in patients that participate in testosterone therapy and may experience shrinkage of the testes; This occurs due to the lack of Testosterone, and sperm production has been shut down in response to the testosterone therapy.
What does post-cycle therapy (PCT) consist of, an example?
Your post-cycle therapy consists of a testosterone secretagogue to stimulate the endogenous testosterone secretion from the testes to reignite natural production. The medication mimics the signal from your brain. The Luteinizing Hormone (LH) induces the production of Testosterone.
For example:
Testosterone secretagogue is human chorionic gonadotropin (hCG), which is administered either using sublingual troches or subcutaneous injections once or twice a week during therapy and then on 10–15 consecutive days as part of a post-cycle therapy (PCT). Human chorionic gonadotropin (hCG) mimics Luteinizing Hormone (LH) to stimulate testosterone production by the testes. It works by effectively tricking the testes into thinking that they are being instructed to produce Testosterone, even though levels are comfortably elevated because of the injectable testosterone therapy.
The testosterone production stimulated by human chorionic gonadotropin (hCG) is insufficient to sustain healthy testosterone levels, but that is not the reason for this supplementation. The purpose is to ensure that the testes remain functioning during therapy to help avoid any shrinkage or atrophy. You will also take an anti-estrogen or aromatase inhibitor.
For example:
Clomid/clomiphene blocks certain types of Estrogen from getting to the pituitary and hypothalamus, where it elicits signals that stop testosterone production. Anti-estrogens or aromatase inhibitors also help reactivate the standard functionality of Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) signaling while helping flush out any residual estrogen accumulated during therapy. The Estrogen that collects during treatment is responsible for many of the adverse side effects of testosterone therapy.
An example of a post-cycle therapy (PCT) protocol is as follows (note that the same drug and dose prescribed will depend on the specific information contained within each patient file, as well as the individual patient goals):
- 250–800 units of a testosterone secretagogue every day for ten consecutive days
- One estrogen blocker or antagonist by mouth every day for 10–15 straight days
Without the proper understanding of what is explicitly occurring within the endocrine system during these crucial weeks, as well as a lack of knowledge of which compounds to utilize, what each compound does, and how to properly use them, serious problems can result.
The Hypothalamic Pituitary Testicular Axis (HPTA)
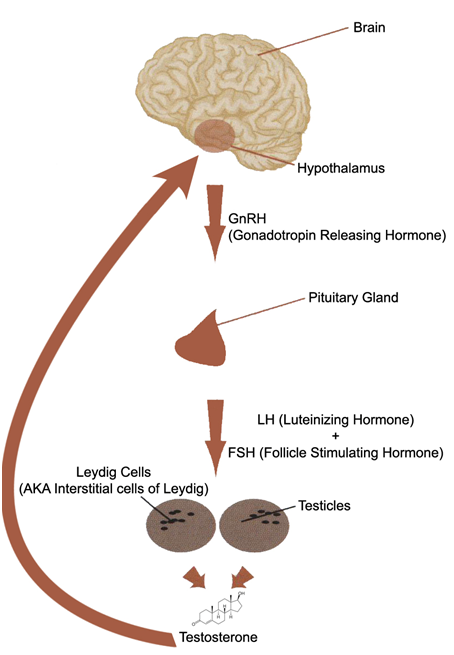
The (HPTA) is an axis interconnected endocrine gland in the body that controls the production of Testosterone. Post-Cycle-therapy: Outlined above is a diagram of the Hypothalamic Pituitary Testicular Axis (HPTA), which Regulates the body and produces the amount of Testosterone at any given time.
Every individual is programmed by (DNA) genetics as to the maximum Testosterone they will provide. The Hypothalamic Pituitary Testicular Axis (HPTA) and the functions that undergo a negative feedback loop, and the body will reduce the secretion of Testosterone, Has too much Testosterone, the body will be detected, known as the negative feedback loop.
This is controlled by the hypothalamus, which is mainly considered the ‘master’ gland for all endocrine systems and the hormonal functions in the body. The negative feedback will loop ultimately in the body to attempt to maintain hormonal homeostasis, and all endocrine glands operate by way of the negative feedback loop in one way or another in varying degrees; in the case of post-cycle therapy, the concern is a negative feedback loop of the (HPTA).
Within the Hypothalamic Pituitary Testicular Axis (HPTA), the concern during post-cycle therapy (PCT) is the restoration and regulation of the following five hormones to homeostasis:
- GnRH (Gonadotropin Releasing Hormone)
- LH (Luteinizing Hormone)
- FSH (Follicle Stimulating Hormone)
- Testosterone production
The Hypothalamic Pituitary Testicular Axis (HPTA), the hypothalamus, which detects a need for the human body to produce more Testosterone, and will release varying amounts of GnRH, Is a hormone that signals the pituitary gland to begin the production and release of two essential gonadotropins: Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH). Two hormones that work together to start the secretion of Testosterone.
Two primary hormonal factors serve to inhibit, reduce, suppress, or shut down Testosterone production in the Hypothalamic Pituitary Testicular Axis (HPTA):
- Testosterone Excess
- Estrogen Excess
Although other hormones exist that inhibit and suppress Hypothalamic Pituitary Testicular Axis (HPTA) function (such as Progestins and Prolactin), these are the two primary conditional hormones of concern. When the hypothalamus detects excess levels of Testosterone and Estrogen in the body (either from the use of exogenous androgens on a testosterone therapy or otherwise), the hypothalamus will act to attempt to restore a balance by essentially doing the opposite of what was previously described.
The hypothalamus will reduce or stop its production of GnRH, which halts the production of Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH), which ultimately reduces or terminates the production of Testosterone. Until the hypothalamus’ ideal hormonal environment is restored, the output of the various signaling hormones within the (HPTA) will not begin, and this will often require months for the body to do this on its own without the intervention of any Testosterone stimulating agents.
The recovery of the (HPTA) naturally takes such a long time should be evident due to the described workings of the (HPTA).
This fundamental understanding of the mechanisms of the Hypothalamic Pituitary Testicular Axis (HPTA) and negative feedback loop described above is essential to understanding how and why a proper post-cycle therapy (PCT) program must be developed and utilized following testosterone therapy.
Determining Factors In Difficulty Recovering the Hypothalamic Pituitary Testicular Axis (HPTA):
With testosterone therapy use, there are several major determining factors in how much difficulty an individual will experience in recovering their Hypothalamic Pituitary Testicular Axis (HPTA) and endogenous Testosterone function during post-cycle therapy (PCT).
They are the following factors, in no particular order of importance:
- Individual response
- Type of Testosterone (s) used
- Length of the cycle (degree of testicular desensitization)
Individual response:
Individuals respond differently to any chemical, compound, Testosterone, food, or drug. While some individuals might experience no Hypothalamic Pituitary Testicular Axis (HPTA) suppression or shutdown at all, other individuals might experience severe Hypothalamic Pituitary Testicular Axis (HPTA) suppression and closure to the extent that they might require far more extended periods to ensure full recovery than most.
Like anything else, this is a spectrum whereby the very ‘lucky’ individuals recover quickly and easily on one end of the spectrum, and the ‘unlucky’ individuals have extreme difficulty recovering during post-cycle therapy. In between the two extremes is the average. Once again, this is due to the individual’s genetic programming as to how the Hypothalamic Pituitary Testicular Axis (HPTA) will respond and attempt to maintain homeostasis.
Type of Testosterone Therapy(s) used
All testosterone therapy exhibit suppression or shutdown of the Hypothalamic Pituitary Testicular Axis (HPTA) through the mechanisms of the negative feedback loop, and there are no exceptions to this. Various testosterone therapy is known as being mildly suppressive, while others are identified as being profoundly suppressive.
This relies on multiple reasons, many of which will not be discussed here. In any case, no matter how mild or severe a testosterone therapy exerts Hypothalamic Pituitary Testicular Axis (HPTA) suppression, all testosterone therapy, when utilized for typical cycle lengths of weeks at a time, will eventually cause the Hypothalamic Pituitary Testicular Axis (HPTA) to shut down, or at the very least severely suppress its hormonal signal processes.
Length of the cycle degree of testicular desensitization
This is the most important and most influential factor. As the range of testosterone therapy use continues, the majority of the Leydig cells of the testes remain dormant and inactive.
The longer these interstitial cells stay dormant and idle, the higher the difficulty is essentially getting these cells to respond to the stimulus of Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) once again. Studies have discovered that the Leydig cells’ recovery following testosterone therapy use is not due to a lack of Luteinizing Hormone (LH) but due instead to the desensitization of the Leydig cells to (LH). In one study in which exogenous Testosterone was administered to male test subjects for 21 weeks, suppressed Luteinizing Hormone (LH) levels were suppressed shortly after beginning administration. However, at the end of the 21 weeks, Luteinizing Hormone (LH) levels were observed to rise within three weeks once the exogenous Testosterone administration stopped. Still, Testosterone levels did not arise until many weeks later in most of the test subjects.
Recovery During The Post Cycle Therapy (PCT).
To stimulate hormonal recovery during post-cycle therapy, individuals must understand that using any medication except for a single select one or two is inadequate for post-cycle treatment (PCT). Ideally, all post-cycle therapy programs should be a multi-component post-cycle therapy (PCT) program that includes several different compounds that work in tandem with one another to provide the most effective and fastest possible Hypothalamic Pituitary Testicular Axis (HPTA) recovery following testosterone therapy.
The three categories of compounds are in order of importance:
- SERMs (Selective Estrogen Receptor Modulators)
- Aromatase Inhibitors
- HCG (Human Chorionic Gonadotropin)
SERMs:
Classes of drugs in the SERM category include Nolvadex (Tamoxifen Citrate), Clomid (Clomiphene Citrate), Raloxifene, and Fareston (Toremifene Citrate). The nature of a SERM is that it exhibits mixed Estrogen agonist and Estrogen antagonist effects on the body. This means that although a SERM might block the development of Estrogen at the cellular level in specific tissues, it can enhance Estrogenic impacts in other areas of the body. These can be positive effects as well as adverse effects. Nolvadex, for example, exhibits Estrogenic agonistic effects in the liver, which is a positive effect, as its effects here result in a positive change in cholesterol profiles (desired by many).
All SERMs, to varying degrees, act as Estrogen antagonists in this area, working to mitigate Estrogen’s effects on breast tissue, reducing or blocking the side effect of gynecomastia. Regarding the impact of SERMs on endogenous Testosterone stimulation, they serve to act as an Estrogen antagonist at the pituitary gland, triggering the release of Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) as a result. Elevated levels of Estrogen in men can and do suppress the output of endogenous Testosterone via the negative feedback loop, leading to hypogonadism. SERMs for this purpose are essential to any post-cycle therapy (PCT) protocol and are not to be excluded under any circumstance. Regardless, however, the sole focus should not be on SERMs.
Aromatase Inhibitors:
These are compounds such as Aromasin (Exemestane), Arimidex (Anastrozole), and Letrozole (Femara). Rather than block the activity of Estrogen at the cellular level in different tissues, aromatase inhibitors (AIs) serve to lower total circulating Estrogen levels in the body by way of inhibiting the aromatase enzyme, which is the enzyme responsible for the conversion of androgens into Estrogen.
The transformation of androgens into Estrogen results in excess Estrogen levels, which, as explained earlier in this article, will trigger the negative feedback loop leading to suppression of Testosterone production. By way of lowering total circulating blood plasma Estrogen levels, AIs will positively engage the negative feedback loop and result in the release of Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) for the manufacture and secretion of more Testosterone.
This is mainly due to the hypothalamus realizing that circulating. Estrogen levels are too low and will attempt to increase circulating levels of Testosterone for a portion of the Testosterone secreted to become aromatized into Estrogen to restore the hormonal balance.
The other importance of aromatase inhibitors is the ability to mitigate the Estrogenic effects of human chorionic gonadotropin (HCG), which will be explained shortly. It is important to note, however, that most aromatase inhibitors do not comply very well with SERMs such as Nolvadex, and those particular choices should be made regarding which AI is used during post-cycle therapy (PCT).
HCG:
Human Chorionic Gonadotropin is, for the most part, a synthetic Luteinizing Hormone (LH). It is a protein hormone manufactured in high amounts by pregnant females that contains a protein subunit that is 100% identical to Luteinizing Hormone (LH). Therefore when administered to men, it will mimic the action of Luteinizing Hormone (LH) in target tissues, such as the testes.
What results in increased Testosterone production via stimulation of the Leydig cells by human chorionic gonadotropin (HCG)?
Human chorionic gonadotropin (HCG) should never be utilized alone, as its nature as a gonadotropin will itself trigger a negative feedback loop whereby once human chorionic gonadotropin (HCG) is used, the pituitary gland will halt the output of Luteinizing Hormone (LH) until human chorionic gonadotropin (HCG) use has discontinued. Therefore, human chorionic gonadotropin (HCG) must be utilized with a SERM and especially an aromatase inhibitor, as human chorionic gonadotropin (HCG) has been demonstrated to increase aromatase activity in the testes, resulting in rising Estrogen levels.
Putting Them Together:
The reader may wonder which compounds to select from the three categories listed and how to use them properly. The answer lies in understanding the properties of each and, in interpreting these properties, how to use them efficiently and appropriately. Human chorionic gonadotropin (HCG): The first item to be examined will be human chorionic gonadotropin (HCG).
Most testosterone therapy users from the 1960s – mid-1980s did not utilize any compounds for hormonal recovery, and the term post-cycle therapy (PCT) did not even exist then.
It was the only compound utilized when human chorionic gonadotropin (HCG) became increasingly popular (circa 1980). Since then, the medical and scientific understanding of such things has increased exponentially, and there should be no reason for any informed and adequately educated individual to utilize human chorionic gonadotropin (HCG) on its own for post-cycle therapy (PCT).
When used with one of the other two categories of compounds (an AI and a SERM), the dynamics change considerably. It has been mentioned that much of the difficulty in recovering the Hypothalamic Pituitary Testicular Axis (HPTA) following testosterone therapy results from Leydig cell desensitization. Human chorionic gonadotropin (HCG) is necessarily an analog of Luteinizing Hormone (LH), and the testes, after prolonged testosterone therapy, would be as equally desensitized to human chorionic gonadotropin (HCG) as they are to Luteinizing Hormone (LH). However, The human body produces Luteinizing Hormone (LH) amounts on its own that is far too inefficient for proper and rapid Testosterone production.
The body’s natural increase of Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH), evidenced by the study referenced earlier in which it was not until three weeks when Luteinizing Hormone (LH) levels only began to reach the standard physiological measurements following the cessation of Testosterone.
Therefore, the body’s natural Luteinizing Hormone (LH) production does not provide a high enough dose for stimulation nor an immediate stimulus to the tests required for the initial increase in Testosterone needed during the post-cycle therapy weeks. Human chorionic gonadotropin (HCG), utilized in a specific manner during the first 1 – 2 weeks of post-cycle therapy (PCT) at a dose of 100-1,500IU every two days, is what allows the individual to provide the testes with a high amount to provide them with a ‘shock’ effect and sustain this shock effect on the Leydig cells of the testes for a sustained period of the first 1 – 2 weeks of post cycle therapy.
Studies have demonstrated the incredible effectiveness of human chorionic gonadotropin (HCG) for this purpose; it has been suggested that human chorionic gonadotropin (HCG) therapy is utilized to treat low Testosterone and hypogonadism. Following this line of thought, the other two compounds (the SERM and the AI) are to be used as supportive compounds for human chorionic gonadotropin (HCG) use in this 1 – 2 week period, and after human chorionic gonadotropin (HCG) discontinued early on in post cycle therapy (PCT), only the SERM is to be used to carry along the hormonal recovery process.
Despite the good news regarding the ability of human chorionic gonadotropin (HCG) to assist in hormonal recovery, there are still two remaining issues to be addressed:
Human chorionic gonadotropin (HCG) causes increased production of aromatase, leading to increased Estrogen levels.
Following the discontinuation of human chorionic gonadotropin (HCG), the body is left with very little endogenous Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) production due to the exogenous administration of human chorionic gonadotropin (HCG).
Aromatase Inhibitors:
Aromasin (Exemestane) Above All Else The first of the two remaining issues to be addressed will be the fact that human chorionic gonadotropin (HCG) will trigger increases in testicular aromatase expression and result in Estrogen increases in the body. It should also be noted that it will cause an increase in testicular progesterone levels. Estrogen rising is, of course, undesirable during post-cycle therapy (PCT), as it has already been explained that Estrogen will trigger suppression of endogenous Testosterone production, and there is no doubt that any individual wishes to encounter Estrogenic side effects during post-cycle therapy (PCT) either. Therefore, the option here is to include an aromatase inhibitor. However, there is a big problem regarding the other two of the three major aromatase inhibitors (Arimidex and Letrozole).
The issue is the fact that in a post-cycle therapy (PCT) program that includes the use of SERMs such as Nolvadex and Clomid, which are known as essential components to a post cycle therapy (PCT) program, Arimidex and Letrozole have direct negative interactions with Nolvadex. The problem here is that Arimidex (or Letrozole) and Nolvadex both directly counteract one another. One study has demonstrated that when Arimidex is utilized with Nolvadex, Nolvadex will decrease the blood plasma concentration of Arimidex (as well as Letrozole, another commonly used aromatase inhibitor).
The conclusion here is that the use of Arimidex or Letrozole with Nolvadex together is a terrible idea and may work together in a post-cycle therapy (PCT) protocol. Aromasin completely circumvents this problem, as it has been demonstrated to have no interactions with Nolvadex, unlike the other two aromatase inhibitors above. In one study, Aromasin displayed no such reduced effectiveness or any reduced blood plasma levels when utilized with Nolvadex. The additional benefit of selecting Aromasin over all other AIs is the fact that Aromasin has been demonstrated in several studies to impact cholesterol profiles in a negative manner far less than other aromatase inhibitors have, wherein one particular review on cancer patients, 24 weeks of Aromasin (Exemestane) administration held no impact on cholesterol profiles.
Some other studies have also demonstrated a nil effect on cholesterol profiles from the use of Aromasin. Although there have also been some studies that have shown a negative impact on cholesterol profiles resulting from Aromasin use, it is evident that there is not as significant or as negatively impacting effect from Aromasin on cholesterol as another aromatase inhibitor. Finally, in addition to these benefits of Aromasin, it is evident that Aromasin holds the ability to increase Testosterone levels in males, as demonstrated by studies.
For example:
One particularly notable study selected 12 healthy young male test subjects who were administered random Aromasin doses of 25mg and 50mg for ten days, and not only was Estrogen suppressed by a significant amount (38%), but Testosterone levels in the test subjects were observed to have increased by an incredible 60%. Following these details, Aromasin would be the best possible aromatase inhibitor of choice to combat the increased aromatase activity caused by human chorionic gonadotropin (HCG). Therefore, Aromasin would then be utilized at a total 25mg daily dose and only while human chorionic gonadotropin (HCG) is used. Once human chorionic gonadotropin (HCG) is discontinued, Aromasin, too, should be halted. The only following issue to cover now is that of stimulating and maintaining proper endogenous Luteinizing Hormone (LH) release to carry recovery along until the body can become self-sufficient once again.
Nolvadex and Clomid:
The question is often asked among the testosterone therapy-using community: Clomid or Nolvadex? Which one is for post-cycle therapy (PCT)? First of all, the best possible addition to human chorionic gonadotropin (HCG) in a post-cycle therapy (PCT) protocol is Nolvadex (Tamoxifen Citrate), as studies have demonstrated that human chorionic gonadotropin (HCG) and Nolvadex utilized together have exhibited a remarkable synergistic effect in terms of stimulating endogenous Testosterone production and that Nolvadex will work to block the desensitization effect on the Leydig cells of the testes caused by high doses of human chorionic gonadotropin (HCG). This is very important because just as too little Luteinizing Hormone (LH) secretion for extended periods can cause desensitization to gonadotropins, too much gonadotropin stimulation (in the form of human chorionic gonadotropin (HCG) or otherwise) will likewise create a desensitization effect.
Secondly, Nolvadex on an mg for mg basis is far more effective than Clomid in stimulating endogenous Testosterone production and is a more cost-effective choice than Clomid.
Studies have demonstrated that 150mg of Clomid (Clomiphene Citrate) daily raised endogenous Testosterone levels of 10 healthy males by approximately 150%. In contrast, incidentally, 20mg of Nolvadex (Tamoxifen Citrate) daily increased endogenous Testosterone levels by the same amount. It is very evident here that Clomid is beneficial for this purpose, but Nolvadex seems to be a more cost-effective choice seeing as though it is more effective than Clomid when compared to mg for mg.
The benefits of Nolvadex over Clomid do not end there – Clomid.
However, it exhibits Estrogen antagonist effects at the pituitary gland as Nolvadex does, which also shows Estrogen agonist effects. What this means is that Clomid will work in varying degrees as an Estrogen at the pituitary gland, triggering the negative feedback loop and reducing the output of Testosterone stimulating gonadotropins, Luteinizing Hormone (LH), and Follicle Stimulating Hormone (FSH).
This is a severe problem during post-cycle therapy, which is a period in which individuals are trying to recover their Hypothalamic Pituitary Testicular Axis (HPTA) function rather than halt it even further. Ideally, one would want a SERM that exhibits almost 100% Estrogen antagonistic effects on the pituitary gland, and Nolvadex is a perfect choice. When it comes to the dosing aspect of Nolvadex, The standard dose for post-cycle therapy (PCT) and for stimulating the release of GnRH (Gonadotropin Releasing Hormone), Luteinizing Hormone (LH), Follicle Stimulating Hormone (FSH), and ultimately Testosterone is that of a single Nolvadex dose of 20 – 40mg daily.
In all studies involving Nolvadex doses used to stimulate endogenous Testosterone production, only 20 – 40mg daily of Nolvadex was utilized, and it has been shown that doubling the amount to 40mg or any higher will not produce any significant difference in endogenous Testosterone secretion. The only reason why many elects to utilize 40mg daily of Nolvadex for the first 1-2 weeks of a post-cycle therapy (PCT) program is to achieve optimal peak blood plasma levels quicker to ensure Hypothalamic Pituitary Testicular Axis (HPTA) recovery faster.
The ideal post-cycle therapy protocol for 4 – 6 weeks Total post-cycle therapy (PCT) time (depending on the recovery ability of the individual): 01) Weeks 1 – 2:
- Human chorionic gonadotropin at 1000iu/E2D.
- Aromasin (Exemestane) at 25mg/day.
- Nolvadex (Tamoxifen Citrate) at 40mg/day. or 02) Weeks 2 – 6: Nolvadex or (Tamoxifen Citrate).
Additional and Optional, Vitamins, Supplements, and Compounds to Aid During post cycle therapy (PCT), Aside from the principal components discussed, various other parts are primarily optional but still very useful for hormonal recovery of the Hypothalamic Pituitary Testicular Axis (HPTA) during the post cycle therapy weeks.
Vitamin B12 Health Benefits, There has been a lot of controversy over whether or not there is indeed a benefit to taking B12 supplements. Some doctors suggest that if a person is not vegan (though probiotics in the gut can produce some B12), they probably get sufficient B12 from the essential foods they are ingesting.
Let us reference some studies:
There is documented research from the Framingham Study suggesting that 40% of all people are deficient in B12. The American Journal of Clinical Nutrition was researched in 2009, and they published a study suggesting close to 6% of U.S. and U.K. residents over 60 are B12 deficient. Another 20% were referenced as “marginal status.” Vitamin B12 Health Benefits has all vitamins’ most multifaceted and prevalent chemical structure.
One area where it differentiates from other vitamins is that it’s the only vitamin that contains a metal commonly referred to as Cobalamin, which is also a universal term for all the various compounds that may have some B12 properties. B12 can improve energy by aiding in thyroid function and cellular methylation; that being said, B12 is not only valuable for supporting healthy energy levels. It is unequivocally essential to life and whole existence. People deficient in B12 will suffer from serious health issues if the problem is not addressed.
What role B12 plays in the following human biological processes:
- Nerve and brain regeneration
- Adrenal gland support
- Male and female reproductive health
- Nutrient absorption
- Red blood cell formation
- Cellular energy
- Memory recall
- DNA synthesis
Here are some of the risks associated with depleted B12 levels are:
- Pernicious anemia
- Migraine headaches
- Macular degeneration
- Tinnitus
- Fatigue (adrenal fatigue and CFS)
- Multiple sclerosis
- Memory loss
- Neuropathy
- Anemia
- Asthma
- Shingles
- Kidney disease
- Depression
**NOTE** The content in this blog is subject to interpretation and is the opinion of the content writer. We do not claim it to be fact. We encourage you to consult a medical doctor before taking any prescribed medications or supplements.
Conclusion
Supporting Hormones health is essential for overall well-being and vitality. By incorporating regular exercise, proper nutrition, adequate sleep, stress management techniques, and IV therapy, you can help maintain optimal testosterone levels and lead a healthy, balanced life. Always consult a healthcare professional before making significant changes to your lifestyle or starting any new treatments to ensure they suit your needs.
At AAI Rejuvenation Clinic, we advise anyone to think seriously about beginning Hormone treatment if there is no medical need for it. However, we will take every precaution to ensure that you read your program’s positive benefits by providing the latest at-home hormonal mouth-swab testing to ensure we are continually monitoring your progress and aware of any adverse side effects. Fill out the Medical History Form, or if you need more information, call us at (866) 224-5698 or (866) AAI-Low-T.
Low Hormone Symptoms
- Motivation
- Sex Drive and Desire
- Depression
- Fatigue
- Erectile Dysfunction
- Cholesterol
- Low Energy
- Memory Loss
- Osteoporosis
- Wounds & Illness
- Muscle Mass
- Sleep Disturbances
- Thyroid Dysfunction
- Weight Gain
]]>